Lung cancer is one of the most common and deadliest forms of cancer worldwide. According to the American Cancer Society, lung cancer accounts for about 25% of all cancer deaths and is the leading cause of cancer-related deaths in both men and women. Treatment options for lung cancer have evolved significantly in recent years, with targeted therapies playing a crucial role in improving patient outcomes. One such target in lung cancer treatment is the epidermal growth factor receptor (EGFR). Understanding the role of EGFR in lung cancer treatment is essential for healthcare professionals and patients alike as it can lead to more effective treatment strategies and better patient outcomes.
What is EGFR?
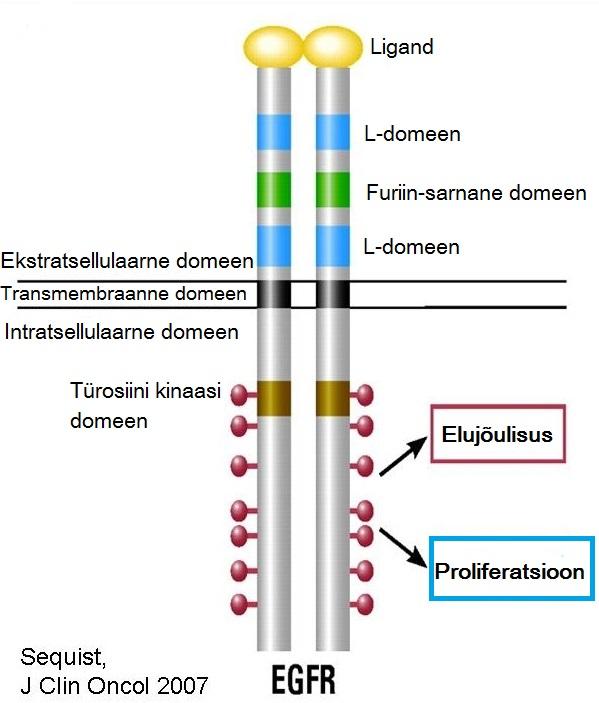
EGFR is a protein that is found on the surface of cells and plays a crucial role in cell growth and division. When activated, EGFR promotes the growth and division of cancer cells, leading to the development and progression of cancer. In some cases of lung cancer, the EGFR gene is mutated, resulting in the overactivation of the EGFR protein. This mutation can lead to the uncontrolled growth and division of cancer cells, making it a promising target for cancer treatment.
The Role of EGFR in Lung Cancer
EGFR mutations are most commonly found in non-small-cell lung cancer (NSCLC), which is the most prevalent form of lung cancer. In fact, about 10-15% of patients with NSCLC have EGFR mutations, making it an important target for treatment. EGFR mutations can lead to the development of aggressive and treatment-resistant tumors, making them challenging to manage with traditional chemotherapy and radiation therapy.
In recent years, targeted therapies that specifically inhibit the activity of EGFR have revolutionized the treatment of EGFR-mutated NSCLC. These therapies, known as EGFR tyrosine kinase inhibitors (TKIs), work by blocking the activity of the mutated EGFR protein, thereby slowing down the growth and spread of cancer cells. This has led to improved outcomes for patients with EGFR-mutated NSCLC, with longer progression-free survival and overall survival compared to traditional chemotherapy.
EGFR Testing in Lung Cancer
Given the importance of EGFR mutations in lung cancer treatment, it is essential for healthcare providers to conduct EGFR testing in patients with NSCLC. EGFR testing involves analyzing a tissue or blood sample for mutations in the EGFR gene. If a patient is found to have an EGFR mutation, they may be a candidate for treatment with EGFR TKIs.
Understanding the role of EGFR in lung cancer treatment is also crucial for patients, as it can help them make informed decisions about their treatment options. Patients with EGFR-mutated NSCLC should discuss EGFR testing with their healthcare providers to determine the most appropriate treatment plan for their specific cancer.
EGFR-Targeted Therapies in Lung Cancer
There are several EGFR-targeted therapies approved for the treatment of EGFR-mutated NSCLC, including first-generation EGFR TKIs such as erlotinib and gefitinib, as well as second-generation EGFR TKIs like afatinib. These drugs have been shown to significantly improve progression-free survival and overall survival in patients with EGFR-mutated NSCLC compared to chemotherapy.
In addition to EGFR TKIs, there are also newer EGFR-targeted therapies available, such as third-generation EGFR TKIs like osimertinib, which have shown even greater efficacy in patients with EGFR-mutated NSCLC. Osimertinib has been shown to significantly improve progression-free survival and overall survival compared to first-generation EGFR TKIs, making it the preferred treatment option for many patients with EGFR-mutated NSCLC.
The Role of EGFR in Treatment Resistance
While EGFR-targeted therapies have significantly improved outcomes for patients with EGFR-mutated NSCLC, treatment resistance remains a significant challenge. Over time, some patients may develop resistance to EGFR TKIs, leading to disease progression and the need for alternative treatment strategies.
Understanding the mechanisms of resistance to EGFR-targeted therapies is an active area of research, with several potential resistance mechanisms identified, including the development of secondary EGFR mutations, activation of alternative signaling pathways, and histological transformation. By understanding these mechanisms, researchers and healthcare providers can develop more effective strategies to overcome resistance to EGFR-targeted therapies and improve patient outcomes.
Combination Therapies for EGFR-Mutated NSCLC
In recent years, the use of combination therapies has emerged as a promising strategy for overcoming resistance to EGFR-targeted therapies in patients with EGFR-mutated NSCLC. Combination therapies may involve the use of EGFR TKIs in combination with other targeted therapies, chemotherapy, or immunotherapy to improve treatment efficacy and delay the development of resistance.
For example, the combination of an EGFR TKI with an anti-angiogenic agent such as bevacizumab has been shown to significantly improve progression-free survival and overall survival in patients with EGFR-mutated NSCLC compared to EGFR TKI alone. Similarly, the combination of an EGFR TKI with chemotherapy has also shown promise in improving outcomes for patients with EGFR-mutated NSCLC.
The Future of EGFR-Targeted Therapies in Lung Cancer
The role of EGFR in lung cancer treatment continues to evolve, with ongoing research and clinical trials focused on further optimizing the use of EGFR-targeted therapies in patients with EGFR-mutated NSCLC. Newer EGFR TKIs with improved efficacy and safety profiles, as well as novel combination therapies, hold promise for improving patient outcomes and overcoming treatment resistance.
In addition, the development of liquid biopsy techniques that allow for the non-invasive detection of EGFR mutations in blood samples is opening up new possibilities for the early detection and monitoring of EGFR-mutated NSCLC. Liquid biopsy-based EGFR testing has the potential to improve patient access to EGFR-targeted therapies and monitor treatment response more effectively, ultimately leading to better outcomes for patients with EGFR-mutated NSCLC.
In conclusion, understanding the role of EGFR in lung cancer treatment is essential for healthcare providers and patients alike. EGFR mutations play a significant role in the development and progression of NSCLC, and targeted therapies that inhibit the activity of EGFR have revolutionized the treatment of EGFR-mutated NSCLC. Ongoing research and clinical trials are focused on further optimizing the use of EGFR-targeted therapies and overcoming treatment resistance, holding promise for improving patient outcomes in the future. By staying informed about the role of EGFR in lung cancer treatment, healthcare providers and patients can work together to develop more effective treatment strategies and improve the lives of those affected by EGFR-mutated NSCLC.












